Hospice patients are prescribed medication to help alleviate certain symptoms and minimize pain at the end of life. These medications should not be taken past the expiration date — for numerous reasons.
The Risks of Expired Medications
Expired medications may be risky or less effective due to potential changes in chemical composition or reduced strength. Some expired medications may have bacterial growth and sub-potent antibiotics that fail to treat infections and may lead to more serious illnesses and antibiotic resistance. There is no guarantee that expired medication is safe and effective for hospice patients who are highly vulnerable to medical complications.
Research suggests that many drug products may have extended shelf lives beyond their expiration date. However, it is difficult for a hospice patient or health care provider to know which medication could have an extended shelf life.
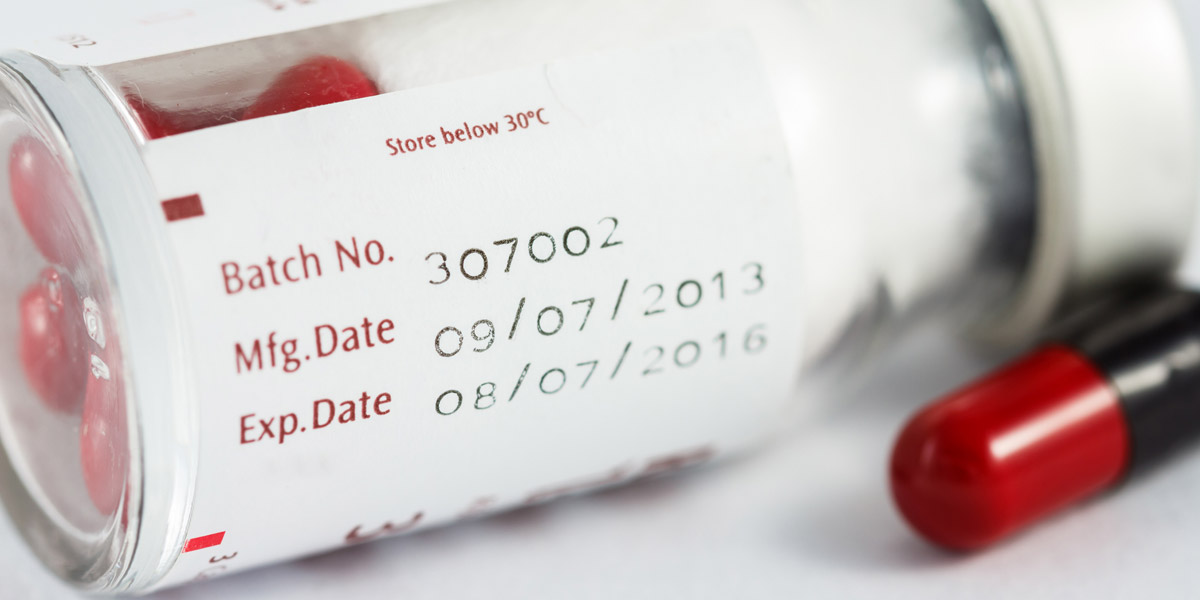
A drug’s ability to have an extended shelf life depends on the actual drug ingredients, presence of preservatives, temperature fluctuations, light, humidity, and other storage conditions. Once a drug is repackaged, the shelf-life could decline due to environmental variations.
How Expiration Dates Are Created
The FDA requires drug makers to provide an expiration date for each medication. Drug makers conduct some testing to determine a drug’s expiration date.
Though extensive testing of drug stability over prolonged periods of time would be ideal, this is often expensive, especially considering that hospice patients keep drugs in very different environments, ranging from hot and cold, to humid and dry. In addition, improvements in drug manufacturing and advancements in drug knowledge over time would require repeated “longevity” testing that could be impractical. Drug makers say it’s better to pick a shorter period of time for drug safety to reduce risk.
However, the pharmacist may reduce the expiration to one year from when the prescription is written. Some states require pharmacists to do this due to a 1985 recommendation from the U.S. Pharmacopeia, a not-for-profit group that establishes standards for drug makers.
The reasoning behind this is that when a drug is removed from its original container and placed in a pharmacy canister, moisture and air can degrade the pills or capsules. In addition, a patient’s condition may change, new drugs may become available, or new information about drug interactions may become available. Thus, limiting hospice prescription medication to a year from when it’s originally filled adds an extra level of safety, requiring the doctor to review a patient’s medications.

How to Dispose of Expired Medication
Hospice patients, or their family members, should read the medicine’s label and follow any specific disposal instructions that may be listed. A drug take-back program, if offered by the hospice pharmacy, is the preferred way to dispose of expired, unwanted, or unused medicine.
If hospice patients don’t have access to a drug take-back program, federal guidelines recommend mixing expired medication with a substance like dirt or car litter, sealing the mixture in a container, and throwing it into the trash.
Certain medications should be flushed down a toilet or sink because they could be very harmful, even fatal, to a child, pet, or hospice patient if taken accidentally.




